Medicine and therefore the history of medicine can be traced back to the earliest human societies. However, this website is about the medical history of Newmarket, which didn’t surface in the historical records as an officially named place until the 13th century (on the parish border between Exning in Suffolk and Woodditton in Cambridgeshire). Moreover, it had no known resident medics until the 17th century (see ‘Henry Veesys etc. – medical care before the 17th century’). Since this page concentrates on how Newmarket medics from the earliest times until the present day fit into and illustrate the history of medicine more generally, it necessarily focuses on medical history relevant to that time frame and geography. However, first it provides some broader context, and discusses some interesting early examples from the wider Newmarket area before the town itself officially existed!
During the medieval period in England (and elsewhere) a distinction developed between three main types of medical practitioner, the physician, surgeon and apothecary. Essentially the physician was supposed to assess the patient and prescribe any treatments required. The apothecary (often part spicer, pepperer or general grocer) would prepare and dispense the medicinal prescriptions, which were mainly compounded herbs and spices (see below for more details). The surgeons were relied upon to carry out most physical treatments – mainly skin and limb etc. (they were often part barber, therefore had the appropriate instruments and skills – again see below for more details). However, these territorial distinctions proved difficult to maintain, and the boundaries were frequently blurred, even in London where attempts to separate the activities of these three types of medic were the most stringent. Certainly in Newmarket a generalist approach has dominated, as illustrated by the account below.
In the earlier medieval period this distinction between different types of medic was less apparent. Essentially someone who practised medicine, in Latin the ‘medicus’ (often translated physician, from the Old French ‘fisiciien’, their equivalent to the Latin word ‘medicus’), used both surgical and medicinal treatments to varying degrees. Part of their therapeutic repertoire would include ‘chirurgia’ (Latin for surgery) derived from the Greek ‘kheir’ (meaning hand) and ‘ergon’ (work) – i.e. work done by the hand. In fact this dual medical/surgical role seems to have been the norm going back to antiquity, since the likes of Hippocrates (c.400 BC) and later Galen (2nd century AD), whose ideas dominated for centuries (although it seems there always have been some who turned their hands just to surgery in its various forms, without strictly speaking being ‘medici’). Galen in particular emphasised the unity of medicine as a discipline, to include surgical treatments. He spent 3 years as a physician to gladiators at Pergamum in modern Turkey, before going to Rome where he became famous for his surgical skills and understanding of anatomy. He also wrote widely on medicinal treatments. In particular he promoted the idea, from ancient Greek medicine, that a balance should be achieved between what medics regarded as the four ‘humours’ of the body: Blood, Phlegm, Yellow bile and Black bile. If they thought that one humour was present in excess it was removed by various means, including what became the very popular practice of blood-letting (seemingly the paracetamol of history!). This was often done by cutting a vein in the arm (see the Home Page of this website for an image), although leeches and some other methods were used for the same purpose. (Interestingly, blood-letting by ‘opening a vein’ is one of the earliest medical interventions recorded in Newmarket, in 1786 by William Sandiver 2, appropriately for Newmarket on the Prince Regent at the races! A physician called in from Cambridge considered it in 1614 for King James I, who’d fallen from his horse in Newmarket, but the king declined. Even as late as the 19th century this practice was still being used – see the pages on Floyd Peck and William Henry Day. The latter in particular has left some very detailed and interesting writings on the subject. As late as 1881 he was suggesting that it was perhaps not such a good idea in children at least – see the page on William Henry Day for more details!)

A monk physician running some tests (see below or click image for source and acknowledgements etc., ref. Image 1).
The training of the very early medieval medics of England is shrouded in mystery, like much in that period. It probably involved a combination of practical training alongside more experienced medics, and the study of ancient texts preserved and also modified/developed in the monasteries during the dark ages. For this reason many medics would have served in monasteries, so potentially leading a beautifully balanced life of prayer, study, contemplation, worship and practical service. There’s a fascinating example of one such ‘medicus’ called Cynefrid, who may well have had links with the area over 500 years before the New-market existed!
Cynefrid was a 7th century physician ‘medicus Cynefridus’ who’s recorded treating Etheldreda, Newmarket’s local saint. Even today the Roman Catholic church in Newmarket and the old hospital chapel are dedicated to St Etheldreda (obviously both so named much more recently, in the light of history). Etheldreda was born in Exning (immediately north-west of Newmarket) in the year 630AD, one of the saintly daughters of Anna, King of the East Angles. What was later to become Newmarket developed on the trading route that runs into East Anglia between the parishes of Exning in Suffolk and Woodditton in Cambridgeshire. In the year 673 Etheldreda founded a monastery at Ely that went on to become present day Ely Cathedral. It’s likely that Cynefrid was a member of Etheldreda’s monastic community (which was for both men and women) – it’s there that he treated her in the year 679. It’s certainly possible that Cynefrid travelled with Etheldreda on occasions to Exning, which is only about 10 miles south-east of Ely. If so, no doubt they would have attended to the physical and spiritual needs of the local population whilst there. Likewise, it’s possible that Exning folk travelled to Ely to seek healing of body and soul, and Cynefrid may well have assessed and treated them. We know from Bede that Cynefrid was still active at least 17 years after the death of Etheldreda. The account of his treatment of her in 679 is recorded in Bede’s Ecclesiastical History of the English People, written only about 50 years after the event. It reads as follows, ‘She had a very great swelling under her jaw [apparently thought to be a plague buboe]. “And I was ordered,” said he [i.e. Cynefrid], “to lay open that swelling, to let out the noxious matter in it, which I did, and she seemed to be somewhat more easy for two days, so that many thought she might recover from her distemper; but the third day the former pains returning, she was soon snatched out of the world, and exchanged all pain and death for everlasting life and health”’. That’s a great example of an early medieval medicus using chirurgia (see above). It’s interesting that he was ‘ordered’ to lay open the swelling – by who? God? Etheldreda? a more senior medic? It’s also fitting that the experience and perspective of the earliest recorded local medic on this website, Cynefrid, obviously resonate with those of Francis Greene 1000 years later, and those of the author of this website just another few hundred years after that (see the Why talkingdust.net? page). Regarding his medicinal repertoire, Cynefrid would also have used various plant remedies such as those recorded in some later Anglo-Saxon herbals. A medieval monastery’s practical work would have involved cultivating herbs for medicinal use.
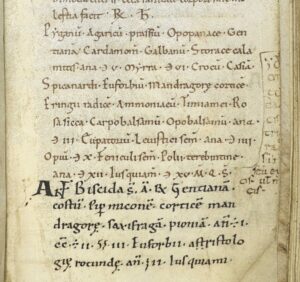
A page from the 11th century medical handbook it’s thought that Baldwin brought with him to Bury. The darker text at the bottom of the page was added by a scribe apparently closely associated with Baldwin, possibly even by Baldwin himself. Note also the use of the medical Rx symbol on the top line shown in this image, still in use today (see below or click image for source and acknowledgements etc., ref. Image 2).
A few centuries later, in Bury St Edmunds (the main town about 12 miles east of Newmarket) there was another very interesting 11th century monk physician named Baldwin. He was born in Chatres in northern France and likely received his medical training at the famous cathedral school there. He worked in various centres before becoming the Abbot at Bury. He’s thought to have brought with him an important medical handbook that he developed during his working life, making various additions (now in the British Library – see image on the left) . It’s been suggested that he perhaps ran what amounted to a medical school for monastic physicians at Bury. He died before the new market emerged from history, but it’s quite possible that early Newmarket residents benefited from the legacy and even services of his institution. Monk physicians like Baldwin, who was physician to the likes of William the Conqueror, would have derived some income from providing medical services to their wealthier patients, and this would have helped fund the monastery’s activities more generally.
About 12 miles to the west of Newmarket is Cambridge, where a little later than Baldwin The Hospital of St John was founded. This was a monastic institution that served the sick, infirm and poor – interestingly essentially integrating health and social care. St John’s Hospital had links with Ely and various places in and around Cambridge. From a Newmarket perspective it’s fascinating that Alexander de Ixnyng (presumably from Exning – his surname likely being descriptive rather than hereditary at that time) was one of the brothers there. Given the role of that institution it seems probable that he was at least in some sense a medic. In 1333 he was elected the Prior/Master of the Hospital (so at the very least he could be described as a Hospital/Practice manager!). Sadly in 1349 he died from the Black Death (presumably as did both of his successors who died that same year – half of the British population died in that 14th century plague epidemic) – see the page on Newmarket and plague.
The monastic training of physicians in the early middle ages gave way to the new universities after the turn of the first millennium. Nearby Cambridge University became established about the same time as Newmarket itself. There was a medical curriculum in both Cambridge and Oxford by the early 14th century, although Cambridge did not have a professor of ‘physic’ i.e. medicine until John Blyth in 1540. The Hospital of St John mentioned in the paragraph above evolved into St John’s college in the early 16th century, having first housed scholars in the 13th century, who left to establish Peterhouse (the first Cambridge college) in 1284. However, university trained physicians were very thin on the ground. In Cambridge, for instance, only one or two medical students were registered each year! No university trained medics practised in Newmarket until the 19th century, aside from those accompanying the royal household like William Harvey.
Surgeons at work in their surgery (see below or click image for source and acknowledgements etc., ref. Image 3).
As mentioned above, increasingly the university educated physicians became less inclined to use surgical techniques, which instead were being carried out by the barber-surgeons. They used their blades etc. to practise surgery (which would have included dressing wounds and ulcers, blood-letting, setting fractures, pulling teeth, incisions, cautery and enemas etc., and some would have performed more ambitious amputations, mastectomies and lithotomy for bladder stones etc.). They were not university trained but served apprenticeships to other barber-surgeons and organized themselves into trade guilds. From the 14th century in London surgeons belonged to the Barbers Company. Then the London Company of Barber Surgeons was established in 1540, but later the Surgeons separated from the Barbers in 1745 to form two separate companies, the surgeons becoming the Royal College of Surgeons in 1800. However, Newmarket medics would have had no links with these London institutions that early. Nevertheless, Newmarket is known to have had at least two barber-surgeons, both in the 17th century, Nicholas Searle and William Raby, although it’s possible there were barber’s performing some surgical procedures in Newmarket earlier. This sort of practitioner was far more numerous than the university trained physicians. Many increasingly dropped hair cutting and essentially became the general practitioners of surgery and medicine for the masses, even in London (although income from mixed sources was common, such as the William Rabys’ barbering, surgery and arable farming – and the taking on of apprentices would have attracted a fee too, as well as providing a handy assistant). During this time the university educated physicians were an elite minority who treated only the rich who could afford their services. In Newmarket the earliest known medical practitioner who likely derived his income primarily from medical services was Richard Greene, chirugian (surgeon), who almost certainly was one of these surgeons with medical repertoire. His apparent younger brother, Robert Greene, obtained a bishop’s licence to practice medicine and surgery in 1617, and likely Robert was apprenticed to Richard, learning both his medical and surgical skills from him (or at least alongside – their father was a grocer, so possibly had a medical repertoire of his own even, from which both learnt? – see comments above and below about grocers). There is no evidence that either of the Greene brothers had a university education. In fact the majority of those licensed in this way to practise in East Anglia were non-graduates. Bishops’ licences to practise had been introduced in 1512 by Henry VIII (sometimes referred to as the 1511 Act, because it was passed in February our 1512, their 1511 – see New Year change). Such licences were granted by the bishop on the testimony of other medics (although Cambridge and Oxford University could already issue licences, and their rights to do this continued; the London College of Physicians could do so as well from 1518, their year of foundation). This licensing system was intended to be universal but many never felt the need to obtain one. Only four Newmarket medics are known to have obtained a bishop’s licence: Robert Greene, Edward Harwell, William Sandiver 1, and Thomas Searancke 2. However, some might have been licensed but the records lost. Apparently this law was not repealed until 1948, so technically anyone practising without a licence before then was breaking the law! – unless perhaps the later commonly held LRCP qualification from the Royal College of Physicians would count (see below)? In effect though this law became obsolete well before the 19th century anyway.

An apothecary at work (see below or click image for source and acknowledgements etc., ref. Image 4).
This not bothering with licences was partly perhaps because another type of medical practitioner had come to the fore during this period – apothecaries, who did not need a licence to ply their trade. Like the barber-surgeons, apothecaries trained via apprenticeships and in cities at least also belonged to trade guilds. In London the apothecaries were part of the Grocer’s company until 1617, when they separated off into their own society. These individuals prepared and sold various commodities including herbs, spices, and medicines/ointments etc. made up from these, which included the use of animal products, and as time went on increasingly they used minerals, metals (which had long been used to some degree anyway) and chemicals. Although they were not supposed to give medical advice but just dispense the prescriptions of physicians, apothecaries did increasingly give medical advice (and use surgical techniques even), not least through necessity in places like Newmarket, given the absence of physicians and the need for a generalist approach. Henry Veesy was a Cambridge based apothecary with links to Newmarket who likely fulfilled such a role (at least giving some medical advice), possibly visiting Newmarket to provide his services in the late 15th and early 16th centuries. Such practitioners faced legal challenges from physicians, but apothecaries won the right to prescribe in the provinces first, then from 1704 in London even. The defence given, even in the earlier cases, was that they were simply doing what apothecaries did. Francis Greene in the mid 17th century is the earliest known Newmarket based medic to use the term apothecary of himself, although given the Greene family’s surgical pedigree in Richard then Robert likely he had a surgical repertoire too. However, it’s also of note that the latters’ father was a grocer, as mentioned above, as early as the mid 16th century (see The Greenes). Francis might have chosen the title apothecary because such medics were becoming increasingly popular, as the opening up of trade with the East and Americas significantly broadened their medicinal repertoire; they were seen as the practical everyday medics, the place to go for some empirical advice and treatment based on jobbing experience. However, the barber-surgeons mentioned in the paragraph above, Nicholas Searle then William Raby, might have largely taken on the surgical work in Newmarket during the time of the later Greenes, i.e. Francis and Lambert.
So this period saw the physician become a rare university educated being who shied away from surgical treatments and the preparation of medicines, alongside the emergence of surgeon-‘physicians’ and apothecary-‘physicians’ to fill the void. And, as described above, in places like Newmarket the distinction was probably blurred, most obviously in Robert Greene, so likely the other Greenes too.
The 17th and 18th centuries saw these two roles merge more obviously into what has become known as the surgeon-apothecary, although Newmarket medics did not use this term – they simply called themselves surgeons and apothecaries, sometimes using one term, sometimes the other, sometimes both. Essentially these were the physicians of the masses, not unlike the original pre-university physicians of old like Cynefrid. They assessed their patients, employing surgical or medicinal remedies as they saw fit. Certainly they were the physicians of the general public in Newmarket. However, since the term ‘physician’ had taken on this more rarefied meaning perhaps the term general practitioner would be more appropriate and what we would call them today, a term first used elsewhere in 1714, not in common use until the 19th century, and not the usual terminology for generalist medics in Newmarket until the 20th century (see below). As already discussed, all of the 16th/17th century Greenes of Newmarket were probably essentially surgeon-apothecary general practitioners in this sense. However, the first Newmarket medic documented to have called himself both surgeon and apothecary was Thomas Searancke 2 in the mid 18th century. The Searanckes were a medical family who started on the apothecary end of the spectrum, ending up very definitely as surgeon-apothecaries by the end of the 18th century. The other main 18th century Newmarket medical family were the Sandivers, who appear to have done the opposite. It appears to have been possible for those calling themselves apothecaries to have apprentices who became surgeon-apothecaries and vice versa without the necessity for dual apprenticeships. The degree of cross training (formal or informal) between those on different ends of the spectrum seems unclear, but there are some documented cases elsewhere of surgeons’ sons being apprenticed to apothecaries and vice versa. Self-education by reading apparently played a significant part too (crucial to any form of education, then as now, supplemented by experience). These all-rounders even started taking on the role of midwives, largely due to the development of instruments like forceps for difficult deliveries, which could be life saving for mother and baby. William Cooke was a Newmarket medic providing services in ‘physic, surgery & laborious or difficult cases of midwifery’ in 1797. William Sandiver 2 was described as a ‘man-midwife’, as was John Edwards, both together in the 1791 Universal British Directory (see the Faint traces page for an image of both of these documents). Sometimes they were called ‘accoucheurs’, later Newmarket examples of this being Frederick Page and George Borwick Mead in 1858. (Incidentally, the earliest mention of a midwife in Newmarket was ‘Johannis Wyote midwyfe’ in the 1413 manor court rolls).
Aside from the general comments above regarding what ‘surgeons and apothecaries’ did, a few interesting examples of their activities in 18th century Newmarket have been preserved. The ‘surgeon’ John Edwards advertised widely his cure for AGUE (fever, especially in the context of malaria), to be used ‘when the Bark [i.e. willow, which contained substances related to aspirin] and all other Medicines have been used without Effect’. He sold this from various outlets across southern and central England. He obviously kept his formula secret (common practice at the time – see the page on John Edwards for further discussion and links). The William Sandivers, aside from their blood-letting activities mentioned above, are recorded as treating syphilis / using mercury (see William Sandiver 1). Both William Sandiver 1 and Thomas Searancke 2 were very active in smallpox inoculation (as opposed to vaccination, which was not introduced until the 19th century- see the page on Newmarket and smallpox).
As mentioned above, before the 19th century the Guild/Company/College of Surgeons, College of Physicians and Society of Apothecaries in London were largely irrelevant in places like Newmarket (Francis Greene had used the Apothecaries’ Arms on his trade tokens, with no evidence that he had any formal link with that organisation; only Thomas Searanke 2 had been a member of the Society of Apothecaries and Thomas Searanke 3 was formally logged there as having started an apprenticeship). Otherwise no pre-19th century Newmarket medics had any links with such institutions, except the visiting physician William Harvey. Officially they only had jurisdiction within a 7 mile radius of London anyway (one mile in the case of the surgeons). Nor is there any evidence that Newmarket medics from this period obtained any training in the London hospitals or medical schools that emerged during the 18th century. This does not however mean that Newmarket medics weren’t trained, just that they weren’t associated with such organisations or officially ‘qualified’ by examination or membership of such institutions. Most would have served apprenticeships of varying degrees of formality, like Walter Norton’s well documented apprenticeship to John Edwards of Newmarket in the early 1780s (see an image on the page about Walter Norton), and William Sandiver 1’s apprenticeship to Wotton Braham earlier that century (see an image on the page about Wotton Braham). Some gained experience/training in the army, then settled into civilian practice (that was possibly the case with Newmarket’s Robert James Peck).
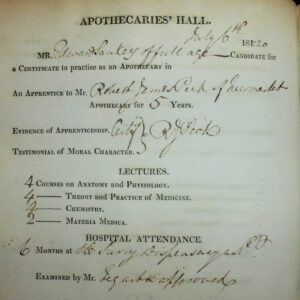
Edward Sankey’s 1820 LSA examination records from the Society of Apothecaries in London, the earliest example of this qualification to be obtained by someone apprenticed to a Newmarket medic, Robert James Peck (see below or click image for source and acknowledgements etc., ref. Image 5).
However, in 1815 there was a major change. The Apothecaries Act of 1815 made it compulsory for all medical practitioners to at least obtain a licence from the Society of Apothecaries in London (gaining the qualification LSA). This required the candidate to serve an apprenticeship for at least 5 years, attend some lectures, and spend some time in a hospital/dispensary, the whole training taking about 7 years typically. The process could begin aged 14 and the minimum age for taking the LSA was 21 years of age. Those already established in practice before the Act were exempt from this requirement. Robert James Peck is an interesting Newmarket example in that regard, having no qualifications himself (see image below), yet being very active in the preparation of apprentices for the LSA examination, including Newmarket’s first medic to obtain that qualification, Edward Sankey in 1820 (see image on the left) – although the first Newmarket medic to actually hold the qualification was Henry Kendall, who gained his LSA in 1819 following an apprenticeship in Spittlefields, London, coming to Newmarket some time between 1819 and 1823 (see an image of his examination records on the page about Henry Kendall). Another of Robert Peck’s apprentices, Michael Minter, left an interesting account detailing the chronology of his training (see the page on Robert James Peck for details). Increasingly it became the norm at the end of an apprenticeship for surgeon-apothecaries to take the Royal College of Surgeon’s membership examination (MRCS) at the same time as the LSA, which became known as ‘going up for College and Hall’ (i.e. Apothecaries’ Hall, as shown on the top of the image above). However, Robert Fyson is a notable 19th century Newmarket example of a surgeon and apothecary who practised on the strength of his LSA alone, yet primarily called himself a surgeon. Conversely, Andrew Ross appears to have been allowed to practice on the strength of his MRCS alone in the late 1820s in his partnership with Robert James Peck as ‘Surgeons and Apothecaries’ (perhaps he didn’t officially function as an apothecary?). Why he didn’t take the LSA examination is unclear, but perhaps it was because he hadn’t served an appropriate apprenticeship, being Scottish where the system was different? Also he was preparing for an MD university degree, which he gained in 1834, so becoming the first Newmarket based medic to hold a university degree – gained after he’d started working in the town. (There was a Mr Nairn, assistant to Norton, Taylor and Kendall in 1828, who had some form of university education, also from Edinburgh, but it’s not clear exactly what – it’s referred to as a diploma.)
Robert James Peck’s entry in the 1847 Medical Directory – note especially that no formal qualifications are mentioned but ‘in practice prior to the Act of 1815, and also note the designation ‘Gen. Pract.’ (see below or click image for source and acknowledgements etc., ref. Image 6).
Alongside these developments, the London medical schools providing the courses and lectures flourished. Initially separate institutions, increasingly these schools became attached to hospitals which provided the experience. As the capacity of these increased the role of ‘dispensaries’ in medical education decreased (dispensaries differed from hospitals in that they didn’t provide inpatient treatment, but some early Newmarket medics gained their ‘hospital’ experience in them, e.g. Charles Edwards, an apprentice of Walter Norton’s who qualified in 1823, and several of Robert James Peck’s apprentices, including Edward Sankey above). Interestingly, the 1841 census captures Floyd Peck in London, aged 21, living in a household with a couple of medical students, yet defining himself as ‘surgeon’. He qualified in 1841, so possibly he’d passed his MRCS at that stage, but the census was in June and he passed the LSA examination in July, so was still with some fellow students (see the page on Floyd Minter Peck for an image of this). His LSA examination records show that his hospital experience was 18 months at St Bartholomew’s Hospital in London.
So the main qualifications that dominated in the 19th century became LSA and MRCS (typcial for a generalist), MD and FRCS (Fellow of the RCS) – typical for the increasingly hospital based specialists in medicine or surgery respectively (for hospital physicians it was not necessary to become a member of the Royal College of Physicians at this stage, unless practising as a physician within a 7 mile radius of London, as mentioned above). Oddly, just as it became compulsory for generalist medics to gain the LSA qualification it seems they largely stopped calling themselves apothecaries, preferring to use the term surgeon, hence GP Surgery, although this trend to prefer surgeon over apothecary can be traced back further, perhaps as an abbreviation for ‘surgeon and apothecary’. As mentioned above, the term General Practitioner only very gradually became the usual job title for generalist medics, becoming the norm during the 20th century, and increasingly making sense as the term surgeon became reserved for the hospital specialists in surgery alone, who with the advent of anaesthesia followed by antisepsis in the mid 19th century started to be able to develop into what we would understand by the term surgeon today. A local early sign of this development was an operation under ether at Bury St Edmunds in 1847 (for details about this interesting event click here). The earliest known uses of the term General Practice/Practitioner in Newmarket were with Robert James Peck and Robert Fyson in 1847 (see the former’s 1847 Medical Directory entry above), and Floyd Peck in 1851. William Henry Day called himself a ‘General Practitioner’ on the 1861 census (see an image of that on the page about William Henry Day), but later moved to London, became a member of the Royal College of Physicians and join the rarefied elite of London consultant physicians! Of course though the term ‘physician’ is still used in two senses even today, of the hospital specialist who is a member of the Royal College of Physicians and specializes in a non-surgical discipline, and in the original more general sense of the local generalist medic, a 20th century example of that being on a memorial to Clement Gray in the pulpit of All Saints’ church, Newmarket, where he’s described as ‘beloved physician’ – see an image on the page about Clement Frederick Gray). Interestingly, the last examples of local GPs describing themselves as surgeons (aside from one or two who actually were modern FRCS surgeons before becoming GPs) come from the Alton House practice in 1944 (but note they were still actually performing significant surgery at that stage – see the page on the Rous Memorial Hospital, including for an image), and Dr Davis and Walden in 1952 (the last known Newmarket example – see the page on Joe Davis for an image). Interestingly though, GPs in the military are still called surgeons. Perhaps the earlier dropping of the term apothecary, and not continuing with that description instead of GP, was partly because the 18th/19th century saw the emergence of the chymist and druggist (later to become the High Street Chemist) whose role was more like that of the traditional apothecary with his shop, i.e. preparing and dispensing medicines more than giving medical advice – but as has always been the case, even now, that distinction was/is blurred at the edges (Chemists give some advice and GPs dispense, preparation now being the realm of pharmaceutical companies, but within living memory GPs and chemists were still preparing some of their own medicines).
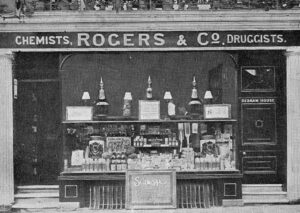
Rogers & Co., early Chemists and Druggists on Newmarket High Street (see below or click image for source and acknowledgements etc., ref. Image 7).
Chymists and Druggists emerged in the 18th century as surgeon-apothecaries concentrated more on clinical practice and less on sourcing and preparing medicines, the demand for which was growing rapidly. Robert James Peck’s parents are an interesting example from Chelmsford (see The Pecks for more details). The earliest known example of the term druggist in Newmarket was with the 18th century Thomas Searancke 2 on the admission of his son to a school at Bury St Edmunds, although primarily he was known as an apothecary and surgeon. George Borwick Mead’s father Joseph Mead, in Ramsey, Huntingdonshire, appears to have been a very late example, i.e. mid 19th century, of this blurred distinction between chemists and medics (see The Meads for more details). The 1823 Pigot’s trade directory lists ‘Peck Robert James’ and ‘Norton, Taylor & Kendall’ under ‘Surgeons and apothecaries’ in Newmarket, but William Cheale and Robert Rogers under ‘Chemists & Druggists’. Intriguingly William Cheale has (druggist only) in brackets after his name – apparently this likely meant that he dealt in medicines derived from organic matter only rather than chemistry – perhaps what we might call a herbalist? The Rogers’ Chemist shop was a feature on the High Street throughout the 19th century, where Greggs bakery is now (see image above). The Newmarket Union poor law minutes record Thomas Dunning, another local chemist, being paid for ‘Chemestry [sic]’ in 1858 (Dunning’s chemist shop can be seen in an image on the page about Mentmore House, which was a couple of doors down the road, although interestingly, by that stage it appears to have been run by someone with a different surname who presumably had kept the old shop name). The history of Chemists in Newmarket is not developed further on this website, since this is the point at which they emerge and diverge from the generalist medical role. Likewise, the history of dentists who emerged in the 19th/20th centuries is not developed further either (apparently in the early 20th century Gilbert Gray was highly skilled at pulling teeth – sadly no longer part of a GP’s repertoire!). However, specialist dental surgeons (dentists) are mentioned visiting Newmarket from the mid 19th century onwards, such as a Mr Jones of Cambridge, who could be consulted at a confectioners shop (!) in the High Street on the first and third Tuesday in the month (according to an advert in the Cambridge Chronicle and University Journal, Saturday 13th June 1857, pg 4).
Regarding what these 19th century medics actually did, the remedies they employed seem very strange to us today. Even quite advanced practitioners for their time used strategies very much like those of the surgeons and apothecaries of the centuries before them. The most eminent Newmarket medic of this period was William Henry Day, whose publications have left us with some wonderfully detailed accounts illustrating the practices of the time (see the page on William Henry Day for more details, especially a case report from 1864 and his later views on leeches and venesection from 1881 already mentioned above, written after he’d moved on to become a London based specialist). The page on the Newmarket Union also includes some examples of what the 19th century medical officers work involved, as do the many pages on this website about individual Newmarket medics from this period (see the ‘People’ navigation tab above, e.g. the page on Walter Hutchinson). Perhaps a few other cases to highlight are Richard Faircloth’s management of a fracture in 1847, with many interesting details, Frederick Page’s resuscitation attempt in 1856, Clement Gray’s extraordinary cæsaerian section case in 1883, and at the turn of the 19th / 20th centuries the ‘typical family doctor’ John Maund’s management of a skull fracture! They really were quite extraordinary all-rounders.
The next major regulatory development that took place following the 1815 Act was in 1858, the formation of the General Medical Council (GMC). This became responsible for overseeing standards of education and producing a register of medical practitioners (The Medical Register). Even now The Medical Register lists all medical practitioners deemed fit to practise by the GMC. When it started, various qualifications were accepted as ‘registerable’, including obviously the LSA, MRCS and MD. In the first edition (published in 1859) there were still some medics allowed to practise with no qualifications at all, on the basis of having been in practice before 1st August 1815 (so they must have been working for well over 40 years). No Newmarket medics were in that category; Robert James Peck had been the last to practise in the town using such criteria; he died in 1848. For a few decades this change made it possible to register and practice as a generalist medic without an LSA qualification, on the strength of an MRCS alone. In Newmarket, John Rowland Wright MRCS 1871 and Walter Hutchinson MRCS 1875 are both examples of that – as was Ernest Fyson’s younger brother Edmund in 1874, who nevertheless added the medical LRCP (a licence from the Royal College of Physicians) to his MRCS in 1882, despite the fact that Ernest had opted for the LSA and MRCS route in 1864/5.
The late 19th and then 20th century saw generalist medics evolve from the local ‘surgeon’, typically with MRCS and LSA, trained largely though apprenticeships to gain these non-university qualifications, into university educated graduates with further postgraduate training and qualifications, essentially specialists in what has become known as Primary Care. This was a gradual process.
First the apprenticeship element waned and the medical school element waxed. The George Meads (Borwick, Owen and Percy) form an interesting example of that in Newmarket (see the page on George Owen Mead for the details). In 1874 it ceased to be compulsory to have served an apprenticeship before taking the LSA examination (apprenticeship ceased altogether in 1892). From 1893 full-time medical education for 5 years became the norm, and from 1886 it had become compulsory for all medical students to be trained in medicine and surgery (and midwifery) before diversifying into becoming physicians, surgeons or GPs after qualification. In time medical schools / teaching hospitals became increasingly university linked.
Despite these developments, it continued to be possible to get onto the medical register and practice as a generalist medic without a university degree until surprisingly recently. In 1884 the Physicians teamed up with the Surgeons to offer what was known as the Conjoint Diploma LRCP MRCS, which became a popular pair of qualifications to register with, Newmarket examples being Ernest Crompton in 1889, John Hansby Maund 1890 and Gilbert Gray in 1908. Likewise in 1886 surgery was introduced into the LSA, which after 1907 was called the LMSSA to reflect that, although there do not appear to have been any examples of Newmarket medics with that particular qualification. It became popular for such medics to style themselves as Physician and Surgeon, Ernest Crompton again being a good example of that in Newmarket, and John Hansby Maund. Gradually more people took the university degrees MB or BM in medicine and BS or BCh in surgery (the first Newmarket example being Norman Gray in 1915, unlike his slightly older brother Gilbert who practised with just his MRCS and LRCP). Joe Davis appears to have been the first Newmarket medic to practise with just his MB and BS degrees. This plethora of qualifications offered by different institutions continued to be acceptable for registration, and as late as 1993 the Physicians, Surgeons and Apothecaries teamed up as the United Examining Board (UEB) to offer the non-university triple qualification LRCP, LRCS, LMSSA. Some took these exams alongside their MB BS as a back-up in case they failed! It wasn’t until 1999 that this means to registration was abolished, so it wasn’t until the 21st century that medics were required to have a degree.
It’s interesting to consider how the adoption of the title Dr by medics fits into this evolving picture, obviously used by people who not only didn’t have a PhD but didn’t have a degree or university education at all! Those with an MD degree (equivalent to a PhD in the British system) obviously could be called Dr, but these were very thin on the ground. They were primarily the hospital physicians in larger towns. The surgeons, generally speaking having served apprenticeships and not having an MD qualification, were known as Mr, even when their practice became more sophisticated in hospitals (which is why today when a medic becomes a surgeon he drops the title Dr and reverts to Mr, keeping up that tradition). Most medics in 19th century Newmarket and before did not have an MD qualification (although few did, interestingly several of whom later became hospital doctors i.e. Andrew Ross, Frederick Page, and William Henry Day). They had trained by apprenticeship, and as outlined above called themselves surgeons, so generally were known as Mr not Dr. A very clear example of the distinction at work in Newmarket is Frederick Gray compared with his son Clement. In the late 19th century they were differentiated as Dr Gray (Frederick, who was unusual in having an MD) and Mr Gray (Clement, who didn’t), for example in the write up of the extraordinary cæsarean section case of 1883 (click here for the full account) and an 1875 reference to them both. However, things were not quite as simple as that, since there had been some tendency to call surgeon/apothecary type medics Dr going back to the 17th century even, so called ‘Dr by the breath of the people’ – the earliest example of that in Newmarket being William Sandiver 1 in the 1740s. However, ‘Mr’ predominated in Newmarket until the 20th century, when it seems to have become the norm for the GPs to be known as ‘Dr’. This was not simply because they started to obtain degrees that could perhaps be regarded as approaching PhD level, with the clinical years added to the basic medical science years. Clement Gray seems primarily to have been called Mr Gray in the 19th century and Dr Gray in the 20th, despite having no change/addition to his LSA MRCS qualifications gained in 1870 following an apprenticeship to his father. A newspaper report about Ernest Last Fyson (LSA, MRCS, LRCP) in 1890 called him Dr, Mr and a surgeon in the same breath (and similarly in 1878 he was called ‘doctor’ Mr and a physician). Interestingly Andrew Ross, as mentioned above the earliest resident Newmarket medic to obtain an MD degree (in 1834) later appears to have written something on ‘The False Assumption of Medical Titles’ by others! Walter Norton was called ‘Dr. Norton’ posthumously as early as 1846, but otherwise was always known as Mr during his career in the late 18th and early 19th centuries.
Alongside these developments in qualifications, scientific developments in medical care obviously transformed the role of medics in the 20th century. What were essentially still the compounded herbs and spices etc. of the apothecary were increasingly replaced by powerful pharmaceutical drugs. As the medical profession became ever more complex and sub-specialised it became increasingly necessary for the generalist medic to ‘consult’ the hospital specialist, who thus became known as a consultant. Everything but minor surgery was taken over by hospital based consultant surgeons. Reflecting this, for several decades after the Second World War Newmarket had its own District General Hospital full of specialists (before the war the workhouse infirmary on that site and the town’s Rous Memorial Hospital had been staffed by the local generalists – see the pages on Newmarket Hospital and the Rous Memorial Hospital for details). Since then Newmarket has been served by specialists based in Bury St Edmunds and Cambridge (see the pages on Referral hospitals and the Newmarket Union, where there are also some examples of how Bury and Cambridge based medics, and those from elsewhere, were sometimes involved with Newmarket patients before the war, even in the 19th century).
So as the 20th century progressed it became increasingly obvious that general practice was not inhabited by medics who could do everything! It had evolved into a speciality in its own right that’s increasingly become known as Primary Care (a much better term than family medicine, which seems inappropriately to exclude people not in families!). Modern GPs, who still prefer to be called GPs rather than primary care specialists, seek to maintain a broad perspective and knowledge that enables them to assess whatever patients care to bring, focusing on the individual as they relate to their various symptoms etc., helping to make sense of them, and proposing solutions that might involve understanding and orchestrating the increasingly diverse repertoire of more specialist services/medics available, provided a simple solution (or no solution) isn’t all that’s required – which is often (perhaps this complex sentence illustrates the complexity of the task!). GPs founded their own college in 1952 (the CGP), which became the royal college, so RCGP, in 1972. The optional post graduate qualification MRCGP (as opposed to MRCP for hospital physicians and MRCS/FRCS for hospital surgeons) was introduced in 1965 (the earliest Newmarket example appears to have been Dr Dossetor of Alton House Surgery in 1966). During the 1960s training schemes started to develop (rotations of junior hospital jobs, passing through a mix of specialities, with some time spent as a trainee in general practice too). These provided some postgraduate training and experience after registration for those wanting to specialise in general practice. In 1976 this ‘vocational training’ as it had become known was made compulsory, then in 2007 gaining the MRCGP qualification became compulsory too for doctors wanting to enter general practice.
Further developments in the 21st century so far have seen tweaks to undergraduate and postgraduate training and registration. The undergraduate course has sought to integrate the pre-clinical sciences and clinical studies more. After graduation it now takes a further 5 years to become a GP (2 years foundation posts and 3 years at registrar grade) – typically it takes at 8 years to become a hospital specialist (2 years foundation posts and then 6 years at registrar grades). The Medical Register now defines doctors as either Specialists or General Practitioners and a system of ongoing annual appraisals with 5 yearly revalidation has been introduced as a requirement to remain registered.
It’s interesting to reflect on the fact that there have always been those who wanted to serve as medics to the people of Newmarket and surrounding area. The treatments, training, qualifications and regulation of these medics has changed, but basically the aspiring medics have simply jumped through whatever hoops were required to get on with the task at hand. Now it’s going to a university based medical school leading to an MB MS degree, followed by postgraduate on the job training leading to an MRCGP qualification, and regulation by the GMC. Not long ago it was apprenticeship to a surgeon-apothecary, attendance at lectures and some time in a hospital leading to the LSA MRCS qualifications, with no such thing as the GMC. Before that it involved a relatively long apprenticeship leading to no formal paper qualifications, but strictly speaking a Bishop’s licence being necessary that few bothered to obtain. etc. etc.
But finally a new brand of generalist medic should be noted, likely to play an increasing role as the 21st century develops – the nurse practitioner. The first mention of a medical nurse in Newmarket appears to have been Mrs Holmes with William Sandiver 1 in 1743 (see an image on the page about William Sandiver 1). The 19th century saw the slowly evolving role of nurses at the workhouse infirmary (see the page on Newmarket Hospital). The Newmarket Union minute books started mentioning District Nursing Associations from 1897, apparently first subscribing to their services in 1904. Then later in the 20th century nurses started to be employed within practices and given the job title Practice Nurses. More recently some of these have undergone extra training in diagnosis and prescribing etc., evolving into what’s become known as Nurse Practitioners. In some ways these versatile medics have even more in common with the totipotent medics of old than modern GPs, in that their repertoire is very broad, with more expertise in vaccination and the dressing of wounds etc. than the average GP, both bread and butter activities for a surgeon-apothecary.
Image 1: From the Wellcome Collection (cropped); image used under CC BY 4.0, reproduced with kind permission of the Wellcome Collection. [Note: click here for the source.]
Image 2: Ms Sloane 1621, f.44 (cropped); image ©, reproduced with kind permission of The British Library Board. [Note: see comments under the Licence T source below as well.]
Image 3: An oil painting by a follower of David Teniers the younger, from the Wellcome Collection (cropped); image used under CC BY 4.0, reproduced with kind permission of the Wellcome Collection. [Note: click here for the source.]
Image 4: ‘The Apothecary’ by Henry Stacy Marks, from the Wellcome Collection (cropped); image used under CC BY 4.0, reproduced with kind permission of the Wellcome Collection. [Note: click here for the source.]
Image 5: From The Society of Apothecaries’ Court of Examiners Candidates’ Qualification Entry Book 1819-1823, reference MS8241/2 (cropped); image ©, reproduced with kind permission of The Society of Apothecaries Archives, London.
Image 6: From a copy of the Medical Directories at The Society of Apothecaries Archives, London; reproduced with kind permission of The Society of Apothecaries Archives. [Note: The Medical Directory. London: Churchill, has been known by various titles over the years. Initially it just covered London, but from 1847 it had a wider remit, being variously known as the London and Provincial Medical Directory, The Medical Directories, The Medical Directory, etc., essentially the same work with minor variations and developments. It is usually referred to as The Medical Directory (as opposed to The Medical Register), so that is how it’s consistently referred to on talkingdust.net.]
Image 7: From Peter Norman’s Collection (cropped); image reproduced with kind permission of Peter Norman.
Note: see comments regarding images and copyright © etc. on the Usage &c. page as well.
Note: For more detailed references relating to specific individuals etc. illustrating points mentioned above, follow the links in the text to other pages on this website.
Anderson S. Making medicines. A brief history of pharmacy and pharmaceuticals. London: Pharmaceutical Press; 2005.
British History Online. Hospitals: St John the Evangelist, Cambridge. http://www.british-history.ac.uk/vch/cambs/vol2/pp303-307 (accessed 28th February 2015).
Burnby JGL. A study of the English apothecary from 1660-1760 (a thesis submitted for the Ph.D. of the University of London.). London: University College; 1979. [Note: this is available to view online at http://discovery.ucl.ac.uk/1349181/1/450256.pdf.]
Digby A. Making a medical living. Cambridge: Cambridge University Press; 1994.
Digby A. The evolution of British General Practice 1850-1948. Oxford: Oxford University Press; 1999.
Duin N, Sutcliffe J. A History of Medicine. London: Simon & Schuster Ltd.; 1992.
Carter EH. The Norwich Subscription Books. A study of the Subscription Books of the Diocese of Norwich 1637-1800. London, Edinburgh, Paris, Melbourne, Toronto and New York: Thomas Nelson & Sons Ltd.; 1937.
Cockayne EE, Stow NJ. Stutter’s Casebook, A junior hospital doctor, 1839-1841. Woodbridge, Suffolk: The Boydell Press, Suffolk Records Society volume XLVIII; 2005. (General introduction, the training of doctors, pg xiii-xvi.)
Conrad LI, Neve M, Nutton V, Porter R, Wear A. The western medical tradition 800 BC to AD 1800. Cambridge University Press; 1995.
Giles JA. The miscellaneous works of venerable Bede in the original Latin collated with the manuscripts and various printed editions, accompanied by a new English translation of the historical works, and a life of the author. London: Whittaker and Co.; 1843. [Note: source for the quote above regarding Cynefrid’s treatment of Ethedreda, Volume 3 (books 4&5), pages 86-89.]
Guy JR. The episcopal licensing of physicians, surgeons and midwives. Bulletin of the history of medicine 1982;56:528-542.
Heasman R (Dick). 160 years of service to the community. A history of Newmarket General Hospital. Mid Anglia Community Health NHS Trust; 1996. [Note: see the page on Newmarket Hospital for further details regarding this reference.]
History behind the RCGP. History of the College. http://www.rcgp.org.uk/about-us/history-heritage-and-archive/history-of-the-college.aspx (first accessed 5th March 2016).
Holloway SWF. The Apothecaries Act, 1815: A reinterpretation. I. The origins of the Act. Medical History 1966;10(2):107-129.
Holloway SWF. The Apothecaries Act, 1815: A reinterpretation. II. The consequences of the Act. Medical History 1966;10(3):221-236.
Irvine S. Surgeons and apothecaries in Suffolk: 1750-1830. PhD thesis. University of East Anglia; 2011. [Note: this is available to view online at www.ueaeprints.uea.ac.uk/36355/1/2011IrvineSPhD.pdf.]
James RR. Licences to practise medicine and surgery issued by the archbishops of Canterbury, 1580-1775. Janus 1937;41:97-106.
Lambeth Palace Library. Lambeth Palace Library Research Guide. Medical Licences Issues by the Archbishop of Canterbury 1535-1775. http://www.lambethpalacelibrary.org/files/Medical_Licences.pdf (accessed 23rd August 2014).
Licence T. Bury St Edmunds and the Norman conquest. Woodbridge: The Boydell Press; 2014. [Note: chapters 10 and 11 of this book, written by Gullick M and Banham D respectively, are my source for the information about Abbot Baldwin’s medical handbook.]
Loudon I. Medical Care and the General Practitioner 1750-1850. Oxford: Oxford University Press; 1986.
May P. Newmarket 500 years ago. Suffolk Institute of Archeology 1975;33(3):253-274.
May P. Newmarket Medieval and Tudor. Published privately; 1982.
May P. The changing face of Newmarket 1600 – 1760. Peter May Publications; 1984. [Note: see comments regarding this and other Peter May material on The Greenes page.], [Note also, see the reference to Peter May’s general research notes below as well.]
Newmarket Manor Court Rolls 1413. Reference: 1476/1/47 (50F/B1 roll 47), also transcript HD1584/45, (Suffolk County Record Office, Bury St Edmunds). [Note: on looking for this reference again in 2019, when considering obtaining an image, roll 47 appears to have gone missing? – if anyone reading this finds it, please let me know (perhaps it’s been misfiled?).]
Newmarket Union Minutes. Reference: 611, (Suffolk County Record Office, Bury St Edmunds). [Note: 611/22, 8th October 1858 for the reference to Thomas Dunning being paid for ‘chemestry [sic]’.]
NHS History. The Development of the London Hospital System. http://www.nhshistory.net/hospitals_and_medical_education.htm (accessed 23rd January 2017).
Nutton V, Porter R. The History of Medical Education in Britain. Amsterdam – Atlanta, GA (USA): Rodopi; 1995.
Online Etymology Dictionary. http://www.etymonline.com/ (accessed 17th September 2014).
Pigot and Co.’s London & provincial new commercial directory, for 1823-4. London: J. Pigot; 1823, pg 172ff.
Poynter FNL. The Evolution of Medical Education in Britain. London: Pitman Medical Publishing Company Ltd.; 1966.
Poynter FNL. The Evolution of Pharmacy in Britain. London: Pitman Medical Publishing Company Ltd.; 1965.
Roberts RS. The personnel and practice of medicine in Tudor and Stuart England. Part 1. The provinces. Medical History 1962;6:363-382.
Roberts RS. The Personnel and practice of medicine in Tudor and Stuart England. Part 2. London. Medical History 1964;8:217-234.
Royal College of Surgeons. History of the College. http://www.rcseng.ac.uk/about/history-of-the-college (first accessed 9th August 2014).
Shaw J. The Newmarket Time Line. Newmarket Local History Society; 2000.
Shops History Newmarket. http://www.newmarketshops.info/index.html (accessed 1st December 2016 re: Rogers Chemist Shop). [Note: newmarketshops.info has been supplied with information regarding the medical history of Newmarket by the author of talkingdust.net since August 2013 (see footnotes on some of the pages). Both websites continue to be developed, and in this sense are mutually symbiotic.]
Sneesby N. Etheldreda, princess, queen, abbess & saint. Haddenham: Fern House; 1999.
Talbot CH, Hammond EA. The medical practitioners in medieval England. London: Wellcome Historical Medical Library; 1965.
The Medical Directory. London: Churchill. [Note: this publication has been known by various titles over the years. Initially it just covered London, but from 1847 it had a wider remit, being variously known as the London and Provincial Medical Directory, The Medical Directories, The Medical Directory, etc., essentially the same work with minor variations and developments. It is usually referred to as The Medical Directory (as opposed to The Medical Register), so that is how it’s consistently referred to on talkingdust.net.]
The research notes of Peter May. Reference: HD1584, (Suffolk County Record Office, Bury St Edmunds). [Note: see the May P. references above also.]
The Worshipful Society of Apothecaries of London. Our History. http://www.apothecaries.org/society/our-history/ (accessed 28th June 2014).
University of Cambridge. About the University – Early records. http://www.cam.ac.uk/about-the-university/history/early-records (accessed 6th September 2014).
University of Cambridge, School of Clinical Medicine. History of the School. http://www.medschl.cam.ac.uk/about/history-of-the-school/ (accessed 9th August 2014).
van Zwanenberg, D. The training and careers of those apprenticed to apothecaries in Suffolk 1815-1858. Medical History 1983;27:139-150.
Voigts LE. Anglo-Saxon plant remedies and the Anglo-Saxons. Isis (The University of Chicago Press) 1979;70(252):250-268.
Thanks also to the many medical historians with whom I’ve had conversations and communications over the years (including attending lectures). They have greatly helped me to develop a general understanding of this subject, such that some of what I’ve included above is derived from that general knowledge and understanding, reinforced by repetition from several sources over time, synthesised by my own reflections on the overall picture, especially from this study of Newmarket.
Note: For published material referenced on this website see the ‘Acknowledgements for resources of published material’ section on the ‘Usage &c.’ page. The sources used for original unpublished documents are noted after each individual reference. Any census records are referenced directly to The National Archives, since images of these are so ubiquitous on microfilm and as digital images that they almost function like published works. Census records are covered by the ‘Open Government Licence’ as should be other such public records (see the ‘Copyright and related issues’ section on the ‘Usage &c.’ page for which references constitute public records, and any other copyright issues more generally such as fair dealing/use etc.).